Abstract
Introduction Minority populations within the United States bear a disproportionate burden of health disparities, which has been demonstrated across studied malignancies. The effect that race plays on treatment access and overall survival (OS) in chronic myeloid leukemia (CML) is poorly understood. Using a large national database, we aim to identify how racial and ethnic identity effects access to treatment and survival outcomes in CML
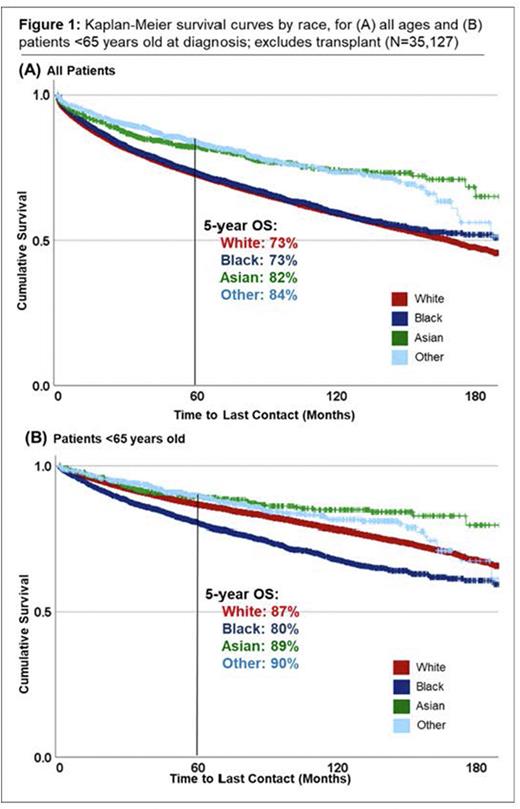
Methods Using the National Cancer Database we identified CML patients (pts) diagnosed from 2004-2019. Demographic and treatment characteristics were compared for White, Black, Asian, Hispanic and other minority populations, with race and ethnicity self-identified by pts. Excluding pts who were managed with upfront allogeneic stem cell transplant, Kaplan Meier and adjusted Cox regression survival analysis were used to compare OS by race and ethnicity, with repeat analysis for the <65 year (yr) old cohort. Multivariable Cox regression was adjusted for age, Charlson-Deyo comorbidity index, sex, insurance, and zip code income and education level quartiles to compare OS by race.
Results We identified 38,763 pts diagnosed with CML, of which 81% (N=17,739) identified as White, 12% (N=4,672) Black, 3% (N=1,125) Asian, and 4% (N=1,422) identified as Other race. 3,304 pts (9%) were Hispanic ethnicity. The median age of all CML pts was 57 yrs (interquartile range [IQR] 44-70), with White pts presenting at an older age (median 59 yrs [IQR 45-71]) than other races, with a median age of 53 yrs [IQR 40-64] in the Black population and a median age in the Asian and Other races of 50 (IQR 35-63). Compared to White pts, Black pts were more likely to reside in low-income zip codes (44% vs. 16% of White pts), be uninsured (11% vs. 6%), insured by Medicaid (19% vs. 8%) and be treated at academic centers (47% vs. 36%). Hispanic pts presented at a younger age (median 46 yrs [IQR 34-59] vs 58 yrs [IQR 45-71 yrs] in the non-Hispanic population), and were more likely to reside in low-income areas (29% vs 19%), be uninsured (21% vs 5%), or Medicaid insured (23% vs 9%), all p<0.001. All races were equally likely to receive disease directed therapy at diagnosis.
The median OS for all CML cases was 14.4 yrs (95% confidence interval (CI) 13.9-14.9), with a 1-, 5- and 10- yr OS of 90%, 73%, and 60%, respectively. The 5-yr OS for both White and Black pts was 73% (p=0.114), with 82% 5-yr OS for Asian pts (p<0.001), and 84% for other races (p<0.001). In pts <65 yrs old, the White population had a 1-, 5- and 10-yr OS of 96%, 87%, and 78%, which was significantly longer than in the Black population, at 94%, 87%, and 78%, p<0.001. On Cox regression adjusted for age, Black race was associated with reduced OS (HR 1.24 [95% CI 1.17-1.31], p<0.001) while pts who identified as either Asian race (HR 0.84 [95% CI 0.73-0.97], p=0.020) or other race (HR 0.79 [95% CI 0.69-0.90], p<0.001) were found to have significantly improved OS, referenced to the White population. On Cox regression adjusted for age, race, ethnicity, comorbidity and socioeconomic features, Black race was not associated with worse outcomes over White race (HR 1.03 [95% CI 0.96-1.10), p=0.378). Asian or Other race, and Hispanic ethnicity were associated with significantly improved OS, with HR 0.82 (95% CI 0.71-0.96), HR 0.79 (95% CI 0.67-0.64) and HR 0.77 (95% CI 0.70-0.85), respectively, all p<0.05. Characteristics associated with reduced OS included age (HR 1.05 [1.05-1.06], p<0.001), increased comorbidity burden (HR 1.32 [0.29-1.35], p<0.001), uninsured status (HR 1.98 [1.78-2.20], p<0.001), Medicaid (HR 2.16 [1.98-2.36], p<0.001), Medicare (HR 1.56 [1.47-1.66], p<0.001), and residing is areas with low income (HR 1.17 [95% CI 1.08-1.27) and low education level (HR 1.19 [95% CI 1.09-1.29]), all p<0.001.
Discussion We present the largest study to date examining the influence of race and ethnicity on OS in CML pts. Despite advances in diagnosis and treatment options over the past decade, pts from traditionally underserved populations, including Black, uninsured, and low-income populations, continue to have reduced OS. Black pts have particularly poor survival when compared to White pts of similar ages, however, when adjusted for socioeconomic features associated with healthcare access, the survival gap improves. This indicates that access to treatment remains a significant barrier in this population, highlighting the need for targeted actions to improve outcomes in this population.
Disclosures
Tantravahi:Karyopharm Therapeutics Inc.,: Research Funding; Karyopharm Therapeutics Inc., Novartis, AbbVie, Incyte: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.